Update on the Coronavirus Situation
Virologists have been collecting data on the current coronavirus outbreak. Currently this bears out my initial analysis.
I wrote this post on the coronavirus situation a few days ago. Since then, some new information on the spread and properties of the virus have come to light. There’s a good summary on Vincent Racaniello’s Virology Blog. Here are some of the most interesting points from that article:
The second implication of the epidemiological observations noted above is that the first infections did not occur on 21 December, as previously reported, but much earlier. The first patient on 1 December was likely infected during November. The virus might have been circulating as early as October, as suggested by evolutionary analysis of genome sequences from multiple patients. The virus could have been causing cases of pneumonia even in November, which were overlooked in the background of this disease observed in winter months. More extensive spread of the virus earlier than previously thought could account for the sudden surge of cases in January.
Preliminary studies based on the first 425 confirmed cases have placed the reproductive index, R0, at 2.2 (range 1.4 to 3.9). The R0 is the number of people, on average, who are infected by a single infected person. In comparison, the R0 for SARS-CoV was about 3. Outbreaks can be halted when the R value is brought to less than 1. Transmissibility is determined by the length of time that a virus-shedding patient has contact with other patients. Rapid identification and isolation of infected patients can shorten this period and lower the R value.
In SARS-CoV infected patients, virus shedding largely coincides with the peak of disease symptoms. Given the severity of the disease, many patients were in hospitals and transmitted the infection there. Consequently patient isolation and infection control were essential for halting the outbreak. There appear to be many more mild infections with 2019-nCoV, and there is greater chance for community spread of infection versus hospital spread. Community acquired infections, such as influenza, pose a great challenge for control. Identifying every infected patient to break the chains of transmission will be difficult.
We do not yet know whether 2019-nCoV is transmitted to other individuals during the incubation period – the time before disease signs and symptoms appear. If it is, it will make control even more difficult. The mean incubation period has been estimated at 5.2 days (range 4.1 to 7.0), supporting the use of a 14-day observation or quarantine period for individuals who have been exposed to infection.
A number of experimental vaccines for 2019-nCoV have been announced, but it is unlikely that they will be available to halt the current outbreak. Antiviral drugs would be useful for treatment of very sick patients. Remdesvir, a nucleotide analog with potent antiviral activity against a wide range of RNA viruses, including ebolaviruses, MERS-CoV, and SARS-CoV, should be tested for efficacy against 2019-CoV. It has been shown to be superior to a combination of lopinavir, ritonavir, and interferon beta, which is being evaluated for treatment of MERS-CoV and 2019-CoV infections in humans. With multiple 2019-nCoV virus isolates available, it will be possible to test other existing antivirals or identify new ones.
The author also compares this new coronavirus to influenza:
The CDC estimates that so far this season (in the USA) there have been at least 15 million influenza illnesses, 140,000 hospitalizations and 8,200 deaths from the disease. There are no travel bans in place to prevent spread of seasonal influenza. Those in place in China, and being considered elsewhere, are an attempt to halt the global spread of 2019-nCoV. I doubt they will be effective, as the virus has already spread to 21 countries outside of China, and it is very difficult to prevent the travel of every infected individual. The question now is how extensive the epidemic will be. Will it reach the extent of pandemic influenza? (in 2009, 60 million cases in the US alone). What will the case fatality rate be? (It was 0.02-0.4% for 2009 H1N1 influenza virus, 9.5% for SARS-CoV.) It is too early to answer these questions, but we learn more every week.
The WHO currently estimates the fatality rate of the virus to be about 2%. But they also stress that it’s too early to tell with much confidence, especially because there seem to be a great number of milder cases that do not get reported.
As you can see, my earlier analysis seems to be borne out by the experts so far. I’ll be interested to see what the results are when all the panic has long died down and some in-depth research has been done, which will take months or possibly years. I’ll keep an eye on this.
→ Comment thread for this post in the Fediverse
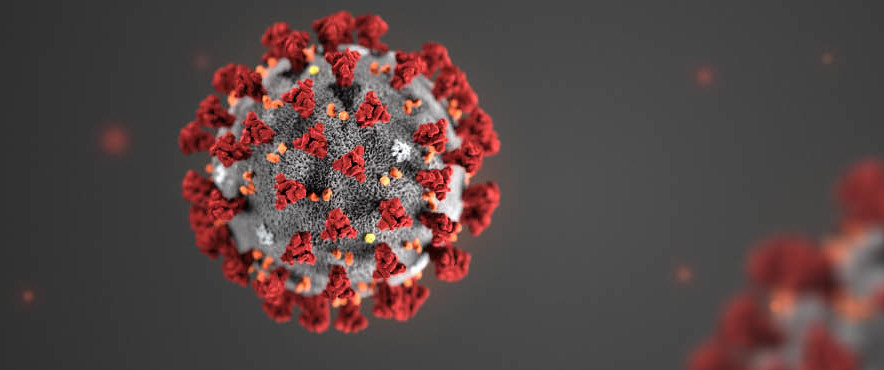
Header image credit: Centers for Disease Control and Prevention